Amsterdam, The Netherlands – Royal Philips (NYSE: PHG, AEX: PHIA), a global leader in health technology, today announced the publication of its Future Health Index (FHI) 2019 report: ‘Transforming healthcare experiences: Exploring the impact of digital health technology on healthcare professionals and patients’ [1]. The report reflects independent research, commissioned by Philips, of what is required to accelerate the shift from volume-based to value-based care in the global drive for sustainable healthcare systems.
Now in its fourth year, the report focuses on the role digital health technology plays in improving both the individual citizen and the healthcare professional experience – two elements of the ‘Quadruple Aim’ in healthcare. The FHI finds that, despite the majority of individuals wanting access to their digital health record (DHR) and being prepared to share it more widely with healthcare professionals, insufficient data sharing currently takes place. This is especially true for data collected by individuals themselves. While around two-fifths of healthcare professionals recommend that patients track health data, such as their blood pressure (44%) or weight (39%), only 9% said that most or all of their patients share this data with them on an ongoing basis.
“Two-way sharing of information is not only essential to deliver the right care at the right time, it also helps to improve the patient and clinician experience,” said Jan Kimpen, Chief Medical Officer for Philips. “Informed and empowered patients also take better care of their health, which contributes to the last element of the Quadruple Aim – lower cost of care. Today’s Future Health Index report highlights that health and healthcare is all about people. For example, the patient-clinician relationship is highly symbiotic. In terms of each party’s well-being, what one side does affects the other and vice versa.”
The Future Health Index 2019 report’s researchers identified three key themes:
1. Engaged and digitally enhanced healthcare professionals
This theme focuses on how healthcare professionals are increasingly using and advocating digital health technology to improve their own experiences. The report highlights that the majority of healthcare professionals are adapting to new ways of working, with 76% reporting that they use digital health records within their hospital/practice, and 80% sharing patient information electronically with other healthcare professionals inside their health facility.
“While many conventional DHRs are often criticized by doctors because of their intrinsic shortcomings, it is encouraging to see that the FHI study shows that the majority of the doctors interviewed still find them useful, so that patient information is readily available to them and ready to share within their hospital,” said Jan Kimpen.
The survey results also point to areas where the full benefits of technology still need to be unlocked.
“Healthcare professionals are rarely prepared in terms of how to use digital technology and data when they’re training for clinical practice,” commented Patricia Mechael, Co-founder and Policy Lead at HealthEnabled and Technical Lead for the Global Digital Health Index. “They may be receiving the latest information when it comes to clinical diagnostics and treatment, but they’re not being trained in the communications and data techniques that they’ll need to use alongside their clinical skills.”
Two-way sharing of information is not only essential to deliver the right care at the right time, it also helps to improve the patient and clinician experience,
Jan Kimpen
Chief Medical Officer for Philips
2. Empowered patients – access to data, more control
The study indicates that giving patients access to their own health data makes them more likely to engage with it in a way that will improve the quality of care they receive and their overall healthcare experience. Of the individuals surveyed, those who share their health data with their healthcare professional are more likely to rate the quality of care as good, very good or excellent (74%) compared to those who don’t share it (66%). In addition, 63% of individuals who currently do not have, or don’t know if they have access to their digital health record, say they want it.
“When patients are more involved in their care, anecdotally we do see better outcomes – they develop a richer and more sophisticated understanding of their health journey,” said Dr. K. Elizabeth Hawk, Clinical Instructor, Stanford University School of Medicine, Department of Radiology, Division of Nuclear Medicine; Radiologist, Matrix Division, Radiology Partners. “Giving patients this access not only empowers them, it also builds a better relationship between physician and patient. And narrowing this disconnect can have a dramatic impact on physician burnout, too.”
“Patients are explicitly asking for access to their digital health records,” said Jan Kimpen. “The benefits are clear. Now is the time for the healthcare industry at large to step up its efforts to really bring patients into the cloud. Other industries have shown that the technology is there to do it in a safe way.”
3. Learning from forerunners
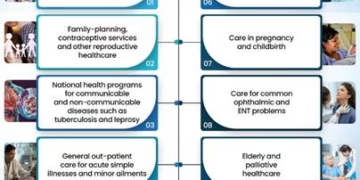
The third theme looks at how some countries have leapfrogged others when it comes to health technology and how digital health technologies are increasingly becoming part of the everyday healthcare experience for both healthcare professionals and patients. For example, the surveyed individuals in China, Saudi Arabia and India more frequently said they take action related to their health as a result of tracking key health indicators via digital health technology or mobile health apps. The experiences of digital health technology forerunners provide lessons that all countries can learn from and apply to their own healthcare systems.
“We know from the previous three editions of the FHI study that it is hard for countries with a developed healthcare system to change, simply because of the legacy,” said Jan Kimpen. “So we should learn from countries with an emerging healthcare system that have leapfrogged in the adoption of digital technologies. Technology is no longer a limiting factor, the important thing for all of us is to be prepared for change.”
Since 2016, Philips has conducted original research to help determine the readiness of countries to address global health challenges and build efficient and effective health systems. Details on the methodology and a full list of sources are available here. To read the full report, visit www.philips.com/futurehealthindex-2019.